Cowper’s Cut 309: The evolution of Tory health policy, from fantasy to shrugging

“When asked about the important issues facing the UK today, the most commonly reported issues were the cost of living (87%), the NHS (84%), the economy (69%), climate change and the environment (58%), housing (57%) and crime (55%).
- Around two-thirds (69%) reported their health was very good or good in general in the latest period; this proportion appears to have gradually decreased since we first started asking about this over time (77% in the period 20 to 30 March 2020).
- Over 4 in 10 adults (45%) who had tried to contact a GP practice in the past month for themselves or others reported finding it easy or very easy to make contact with their GP practice; this proportion has generally remained relatively similar since we started asking about this in May 2023.
- Around 6 in 10 adults (60%) who had tried to contact a GP practice in the past month for themselves or others reported having a very good or fairly good experience of their GP practice; this proportion has remained relatively similar since we started asking about this in May 2023.”
Dying governments reach a point on the pathway where they can do no right.
Many readers will remember this from the tail-end of the Major administration in 1996-7, and that of the Brown administration in 2009-10.

It was telling that in the launch process for this week’s dental initiative, the Gentle Dental practice that PM Rishi ‘The Brand’ Sunak visited is not actually accepting new adult NHS patients, as The Mirror revealed.
At a superficial level, you can ‘so what?’ this. But it’s lazy research by the team around the PM and the Department For Health But Social Care. This failure to do some really basic checking is emblematic of the shrugging sloppiness that characterises the Sunak administration’s approach to public services.
Thank you @PaddyMcGuinness.
— BDA (@TheBDA) February 8, 2024
You really didn’t get it wrong.
You captured the absurdity of a system that’s fuelling a crisis hurting millions.
The PM promised to ‘restore’ NHS dentistry.
We’re still waiting…
SIGN & SHARE this petition to Rishi Sunak. https://t.co/2FfPt0VagG pic.twitter.com/7iIzNuP8wm
Dentistry’s payment perverse incentive technicalities (Units of Dental Activity) made it onto the generally-unwatchable BBC Question Time, via TV presenter Paddy McGuinness. Health policy, eh? It gets everywhere.
Health But Social Care Secretary Until The Next Reshuffle Victoria Atkins was asked by an ITV reporter about a person who claimed they had pulled out twelve of their own teeth due to inability to access an NHS dentist.
ITV News has spoken to a patient who was in so much pain she pulled out 12 of her own teeth with pliers because she couldn't get an NHS dentist.
— ITV News Politics (@ITVNewsPolitics) February 7, 2024
'Somebody in that amount of pain must always remember that if they need to they can go to their local A&E,' the health secretary says pic.twitter.com/I6OS8d1N3K
Atkins replied that that “somebody in that amount of pain must always remember that if they need to, they can go to their local A&E”.
Mmmmmmmm. Mrs Atkins doesn’t seem to be stupid, and is relatively new in post. So we can probably be charitable to her, and put this down to appallingly inept and insouciant briefing.
But, as the Kiss post linked above notes, “the NHS Accident & Emergency service does not treat dental patients unless there is a severe infection that could be life threatening by affecting breathing, swallowing or speech”.
Missed target

In an uncharacteristic and perhaps inadvertent moment of political cunning, the PM’s Monday interview admitting the wildly obvious fact that his 2023 pledge to cut NHS waiting lists had failed was given to Piers Morgan on Talk TV, thus ensuring that virtually nobody would watch it.
Smart, eh? They don’t pay Team Sunak the big Euros for nothing.

Alas! The pesky UK media must be most of the audience for Talk TV (if only through schadenfreude), and so news of the PM’s conceding incompetence-meets-intransigence-driven defeat leaked out quite promptly on media outlets with actual readers and viewers.
In a moment of exquisite political bathos, Sunak told Morgan that “industrial action has had an impact”. One must have a heart of stone not to laugh.
Irony while the strike’s hot
The BMA Junior Doctors Committee announced their latest five-day strike, which is set to run from 24-29 February.

Messages on Kiss (formerly Twitter) from JDC co-lead Vivek Trivedi outlined how these latest strikes follow the Government’s having, he suggests, “failed to table a new pay offer”, which could have been put to members.
We even suggested delaying this action, with the aim to resolve this year’s dispute,
— Vivek Trivedi (@_VivekTrivedi) February 9, 2024
If the government agreed to extend our mandate for a short time to allow space for progress.
If we’d have reached a deal, then the ‘delayed’ strikes wouldn’t be called for at all
Gov said no
The statement from SOS Atkins likewise indicated scant appetite for transigence: she asserted that “this action called by the BMA Junior Doctor Committee does not signal that they are ready to be reasonable”.
My statement on Junior Doctors calling further strike dates. pic.twitter.com/UtzdUxzwJH
— Victoria Atkins (@VictoriaAtkins) February 9, 2024
Ms Atkins further claimed that her side “were prepared to go further” than the previous offer, and “we urged them to put an offer to their members, but they refused”. There is clearly no agreement over the basic fact of whether a new offer was made
So there will be yet more cancellations, disruption and waste. Likewise, there will be cover-related earning opportunities for those consultants who haven’t already booked their skiing trips for that period.
It’s interesting that the BMA JDC leaders have again gone for the ‘block of days’ approach, rather than seeding individual days across February’s remaining weeks (their strike mandate expires on 29 February, although another following mandate looks like a gimme).
I remain of the view that while this is evidently a dispute over pay and conditions, there is an important secondary aspect to this relating to traumas experienced during these people’s work during the pandemic. And I think that this is likewise a driver among consultants and SAS doctors.
I go back to the powerful words of a senior nurse in a regional district general hospital to Professor Kevin Fong (who was there looking at how the system could be recovered after Covid): “you’re all very clever people and I’m sure you’ll come up with very clever things - but what I want to know is, how are you going to recover us? Because we are broken.”
As Isabel Hardman noted in The Spectator ‘Evening Blend’ email this week, resolving this industrial action over pay looks increasingly like it’s going to become another unwelcome item on an incoming Labour government’s epic ‘to do’ list.
The evolution of Tory health policy: from fantasy to shrugging
The Conservative And Unionist Party government led by Rishi Sunak certainly appears to have given up on the NHS.
I had not hitherto thought that ‘shrugging’ would be a part of health policy, but it seems to have replaced the ‘fantasy’ approach of the Johnson administration, best encapsulated by the ‘world-beating’ promises about handling the pandemic and the 40/48 projects of the New (If Fictional) Hospitals Programme.
The shrug is clearly infectious. At The Spectator’s Health Summit this week, NHS England’s director of [cough] strategy Chris Hopson was on a panel chaired by Isabel Hardman, who (channeling the £1,000 Rwanda flights bet between Piers Morgan and the PM) asked Hopson of the productivity targets of 1.5-2% in The NHS Workforce Plan, “will you bet me a pint that you are going to meet them?”
Hopson’s reply was a verbal shrug: “who knows?”
This came after Chris’ unimprovable comments that “NHS England has three priorities. These three priorities are:
- Recover from Covid - Urgent and Emergency Care performance; elective; cancer; access to GP. We are making progress. Then mental health, dentistry, maternity, and recovering productivity lost over Covid.
- Develop NHS ability to reshape and adapt for a new generation. Transforming services, as called for in the Times Health Commission and the BMJ Commission. There’s consensus around the need to change. Digital integral to this, as is moving care closer to home, as is prevention. There is a revolution coming in 21st century medicine. Data.
- The physical infrastructure, and workforce growth and reform.”
These three priorities are a bucket-list of absolutely everything. It is, quite literally, ‘Everything Everywhere All At Once’. Who says NHS England can’t prioritise, eh?
Now that’s what I call [cough] strategy.
No deal: the PM’s choice?

This piece by The Guardian’s Denis Campbell and Pippa Crerar reports on un-named sources who allege that PM Rishi ‘The Brand’ Sunak has been the blocking force preventing a pay deal with doctors being struck.
The piece says that PM Sunak “has been accused of personally holding up a deal to end doctors’ strikes in England despite warnings from the health department and NHS England that waiting lists will continue to soar unless the industrial dispute is resolved.
“… it had been made “abundantly and repeatedly” clear to the prime minister that there would be no progress on his pledge to drive down NHS waiting lists until a deal was struck”.
Mmmmmm. The article makes it clear that the source is either in the Department For Health But Social Care or NHS England. So it’s NHS England, and it’s very likely to be their director of [cough] strategy Chris Hopson. This off-piste, rather obvious briefing is very much Hopson’s choice, in my experience (and yes, I am the person who taught Chris how to use Twitter). The phrase “abundantly and repeatedly” is particulary Hopsonian.
Why did he do this? Chris is shrewd enough to see that one of the very few political options left to the Government which might leave them looking less red-handed would be to first blame, and then sack, senior leaders in NHS England. So you get your retaliation in first.
No doubt there will be more such anonym-ish salvoes in The Sack Race before too long.
The performance fiasco
The data day this week saw another chapter written in the Book of Revelations of The Mundane Apocalypse.
There are so many depressing facts here. Yes, there was a minuscule reduction in the overall RTT waiting list, with 7.6 million entries at the end of December 2023, a slight fall from 7.61 million at the end of November 2023. In January 2023, then PM Sunak made his failed pledge, the RTT waiting list stood at 7.21 million.
There was more nanotechnology-scale good news with 70.3 per cent of patients in England being seen within four hours in A&Es in January 2024 (up from 69.4 per cent in December 2023).
But.
The number of patients waiting for more than 12 hours in A&Es in the NHS in England rose by almost 25% in January 2o24. This was up from 44,045 in December 2023, which was the second-highest figure on record (the winner being the 54,573 recorded in December 2022).

And we know about the clinical risks of long A&E waits.
What about the longest elective RTT waits, the main subject of NHS England’s electoral recovery plan “to boost capacity and give choice to patients”?
Ahem.
Two-year waits rose by 55 patient pathways to 282; over 18-month rose 2,000 to 13,000. As Insource’s Dr Rob Findlay noted, “both should have been eliminated by now. Over 15-month waits rose 4,000 to 98,000: the national target is to eliminate these by the end of March 2024”.

Rob’s usual thorough analysis for Health Service Journal is here.
As I reported earlier this month, the number of people waiting +12 hours on a hospital trolley for an emergency bed was 3,000 times higher in 2023 than in 2011.
— Georgina Lee (@lee_georgina) February 8, 2024
Read my @FactCheck analysis here:https://t.co/bQHpG2ENlW
Channel Four News Fact Check editor Georgina Lee pointed out that in January 2011, just 17 people had faced a wait of 12 hours.
And Liam Thorp of the Liverpool Echo observed that “in January 2015 it (the number of 12-hour A&E waiters) had risen from 17 to 650, and to 2847 in January 2020. January 2024’s number of people waiting over 12 hours in A&E works out as nearly 3,200 times greater than January 2011. A&E attendance increased by 29% in that time”.
The data is compelling, but the human costs are profound.

When in doubt, cheat
If the Department For Health But Social Care and its wholly-owned subsidiary NHS England were to have anything as coherent as a motto, it would probably be ‘when in doubt, cheat’.
This revealed preference became ever clearer this week, as several things picked up by the hardworking HSJ team show. James Illman spotted that changes to administrative process for the 78-week RTT waiting cohort “mean the vast majority of East and North Hertfordshire Trust’s 1,058 cases which have breached 78-weeks will be transferred to a lower profile community services waiting list instead.
“This means the trust will no longer have to declare them as 78-week breaches on its monthly RTT list, which is the primary means of holding trusts and the wider NHS to account on elective care”.

James also reported that “NHS England is in negotiations with ministers to formally push back the target to eliminate 65-week waiters … Discussions about the target are on-going as part of negotiations around the delayed 2024-25 planning guidance. It has been clear for months the March deadline to virtually eliminate 65-week waiters would be missed.
“It has emerged some trusts with the largest waiting lists already appear to be working to a September deadline”.
It’s classic stuff. When a target is about to be missed, change the metrics.

Perhaps the most important trickery was disclosed by Dave West’s exclusive report that the DHBSC-hosted Office for Health Improvement and Disparities is being disbanded. OHID replaced (sort of) Public Health England, but on a less independent basis.
DHBSC “scrapped the previous post of director general for OHID, which represented the unit at the highest level and oversaw all its officials. Jonathan Marron, who held that role, has now been rebadged as DG for “primary care and prevention”.
“… sources said OHID’s teams had also been significantly cut. DHSC has not confirmed the number of reductions, but several people said reductions were as high as 40-50 per cent, with several key director roles lost”.
Well, it’s only public health and prevention. Who needs those? Dave’s analysis of the impact of these changes is a key read.
Jenkinswatch
Writing and reading about health policy and politics can be a gloomy business, in this era of The Mundane Apocalypse. So it was a qualified joy to spot the perennially-wrong-about-everything Simon Jenkins having another go at writing about the NHS for The Guardian.

As public policy commentators go, Jenkins has some knowledge of historical buildings. His piece is sublime (if not sublemon) in its afactual nature: it contends that doctors should not be involved in plans to improve and reform the NHS. Yes, it is indeed a niche view.
Jenkins asserts that he “recently asked two wise doctors, senior in their profession, what was wrong with today’s NHS. Was it money? Was it recruitment, or pay, or structure? Without consulting each other, they answered what was wrong in one voice: “Us”.” I doubt whether I’m alone in wondering whether these two conveniently consensual doctors were members of the reality-based community, or rather representatives of the fictional milieu of inexpert commentators.
I hope this analytical tour de farce will cause a wry smile to play around the corners of your well-chiselled features, as it did to mine. There is a lot of bad commentary on the NHS around: hard as it may be to ignore, usually that’s the most rewarding choice.
But this piece is exceptional in its lack of merit. It is a masterpiece of nonsense, assertion, misdirection and simple bullshit: an index of just how poor commentary in The Guardian has become.
Simon Jenkins is to public policy commentary what Nigel Farage is to ballet.
Monewatch
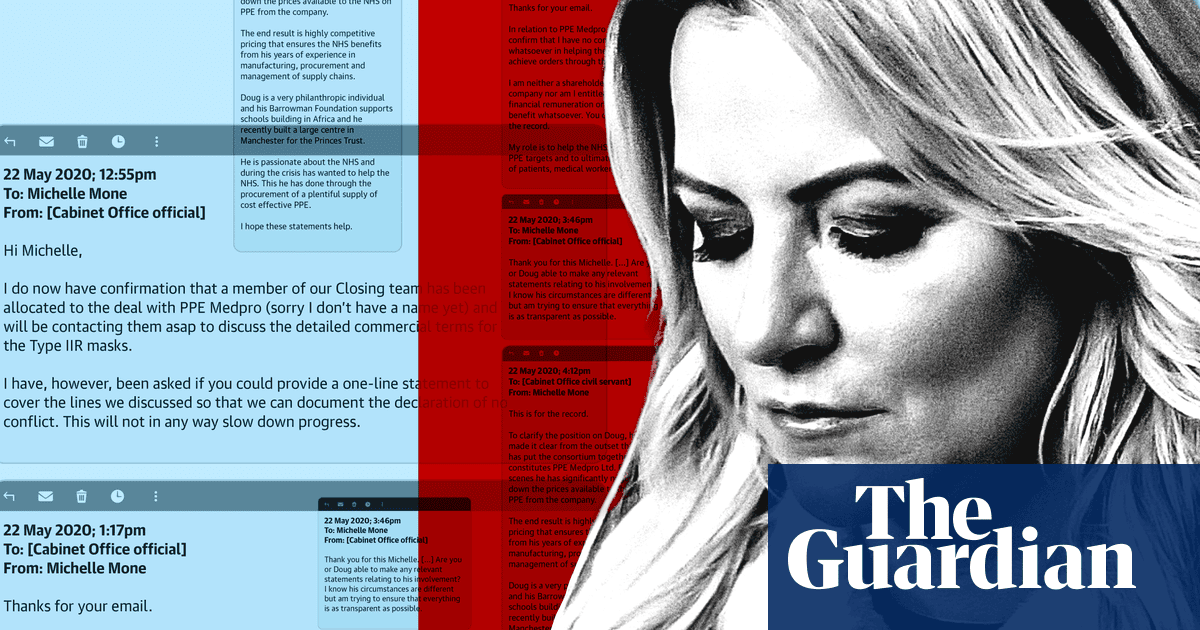
Everybody’s New Favourite Noble Baroness, Tory peer and nominative determinist queen Michelle Mone this week yet again hit the news with aplomb (possibly, even several plombs) for her part in the VIP fast-lane PPE Medpro affair, which is currently under active investigation by the National Crime Agency and the subject of government litigation.
The Guardian’s David Conn was leaked emails between ENFNB Mone and the Cabinet Office, one of whose civil servants was sufficiently old-school to do their actual job and check for conflicts of interest.
The civil servant “asked her to make a declaration that she had no conflict of interest in relation to the company, PPE Medpro, which she had recommended to ministers in May 2020. Mone stated that she had “no conflicts whatsoever” and that she was not “entitled to any financial remuneration or financial benefit whatsoever”.
“The civil servant then asked for clarification about the involvement of Mone’s husband, the Isle of Man-based financial services businessman Doug Barrowman. She replied that “Doug is a very philanthropic individual” who “wanted to help the NHS” and was negotiating to lower the prices the government was paying for PPE.”
— Lady Michelle Mone (@MichelleMone) November 24, 2022
Ooops.
The Alan comeuppance
The People’s Partridge has been unusually, worryingly quiet for some time now. But you can’t keep a good man down, nor can you keep down Matt ‘Alan’ Hancock, who appeared in karaoke fan and senior Number 10 civil servant Helen MacNamara’s lengthy Times interview.
Of The People’s Partridge’s famous boosterism, MacNamara says, “it would have been helpful to have a bit more candour and honesty about the fact that there were problems rather than project those extraordinary levels of confidence into internal meetings”.
Recommended and required reading
Isabel Hardman’s excellent NHS book ‘Fighting For Life’ is now out in paperback.
The Times Health Commission’s main report is here. It means well, but has little or nothing on the practical methods needed to deliver short-term improvement.
The BMJ Commission On The Future of The NHS has started to publish its output here. It, too, means well, but has little or nothing on the practical methods needed to deliver short-term improvement.