Cowper’s Cut 328: Mentioning the whole money thing


Last week’s manifestos coverage meant that I didn’t feature the impressive analysis by Sally Gainsbury for the Nuffield Trust on the main parties’ NHS spending plans.
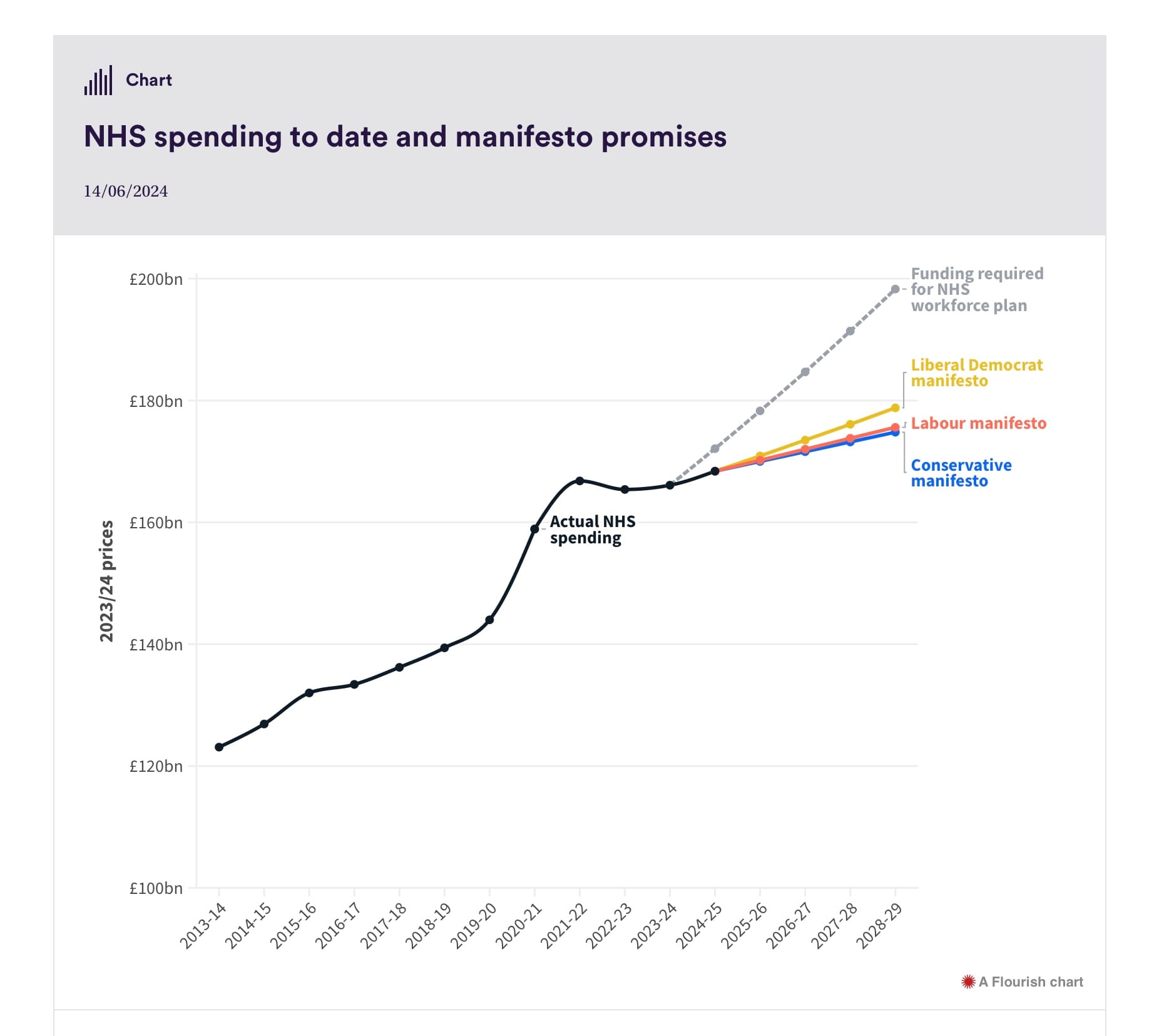
The picture painted by the above graph is bleak - and the funding officially required for the NHS workforce plan is not particularly credible, as the Institute for Fiscal Studies’ analysis noted.
As Sally’s piece concludes, “if any of the three parties’ pledges were implemented, the period 2022/23 to 2028/29 would see the tightest and most sustained NHS funding squeeze in recorded history (going back to 1979/80), resulting in annual real terms increases of just 0.4% under the Conservative pledges, 0.5% under the Labour pledges and 0.7% under the Liberal Democrat pledges: all below the most recent rate of population growth, even before adjusting for the increased health care need of an ageing population”.

Further analysis from the Health Foundation REAL Centre adds to the picture: they conclude that the NHS may need an extra £38 billion over the next decade, above the sums implicitly planned.
The HF approach explores “two scenarios for funding the NHS in England over the next 10 years. The first would meet future care needs and achieve a sustained improvement in services broadly in line with current policy ambitions and public expectations. The second would also meet future care needs but assumes minimal changes to services.
“Achieving sustained improvement would require average annual real-terms funding growth of 3.8% over the next 10 years, with a higher rate of growth during the first 5 years, and a lower rate in the remaining 5 years. This is broadly in line with the historic average growth rate in total health care funding.
“… The minimal change scenario would require average annual real terms funding growth of 2.9%, which is below the long-term historic average. This scenario would see less investment in capital and public health, lower productivity growth, and would not provide all the care needed to clear the backlog.
“Projected spending growth in our scenarios is above that based on the spending plans in line with Office for Budget Responsibility (OBR) assumptions (0.8%). Real-terms funding increases of 0.8% a year up to 2029/30 would leave England’s health care system around £38bn a year short of the spending we project in our sustained improvement scenario.”
Mentioning the NHS need for more money feels a bit gauche, at a point when virtually every part of the public realm is crumbling. We know that Shadow Chancellor Rachel Reeves has emphasised time and again that there can be no uncosted spending commitments, and that the main three taxes (income, NI and VAT) will not increase under her tenure.
Not everything that needs to change in the NHS requires more money, although some areas (most notably, budgets for capital, maintenance and management) clearly do. There is also the issue of contested medical pay deals: see below.
Victoria Atkins is going down fibbing
My response to letter from @TheBMA Junior Doctors Committee 👇
— Victoria Atkins (@VictoriaAtkins) June 20, 2024
These planned strikes are cynical and will harm patients. The BMA must call them off. pic.twitter.com/YHGIRHzgcR
Bob The Whippet’s Emotional Support Human and Secretary Of State For Just Under Three More Weeks Victoria Atkins is determined to go down fibbing, rather than fighting. Bless.
She published a letter to the BMA junior doctors’ committee leadership, which asserts that “if we are re-elected on 4 July, we commit to getting back into the negotiating room immediately”.

Perhaps the strain of supporting Bob’s emotional needs is getting to Mrs Atkins: but as the Government’s own press release makes amply clear, she has not been in the negotiating room.

The junior doctors have responded, telling Times health editor Eleanor Hayward that they “could not rule out” balloting to extend their mandate for industrial action to cover this coming winter, in the absence of a satisfactory pay offer from the incoming government.
They re-emphasised that a deal on their objective of the 35% ‘full pay restoration’ could be staged across a number of years. In this interview, BMA JDC co-lead Vivek Trivedi repeated his assertion (covered in the last ‘Cut’) that Secretary Of State Atkins had told them that she cared “more about what the Daily Mail readership would think and how to explain it on GB News” than finding a deal.
Moves to settle junior doctors’ pay row were deliberately Sunakered
Trivedi told The Times that when Mrs Atkins took office in November “there seemed to be a genuine sense of wanting to try and reach a resolution”, but added: “In our more recent meetings, her behaviour has been very difficult to explain.”
“It’s always been Rishi Sunak’s call. He just has no willingness to come to a deal. I’ve come to the conclusion he instructed Victoria Atkins to put up these roadblocks during the latter period.”
Speaking on Ali Miraj’s LBC radio show, Mr Trivedi carefully emphasised that the last actual offer of a pay settlement was made in December 2023, and that although Victoria Atkins then stated that an improved offer was on its way, it has never in reality been made.
The Times feature also quotes Labour shadow health secretary Wes Streeting: “the BMA should call off the strikes next week and prepare to negotiate with a Labour government. If Labour is elected, the junior doctors will be one of my first calls on 5 July, and we will get talks up and running as quickly as possible to bring an end to this disruption. Patients can’t take any more.
“Rishi Sunak has cynically refused to negotiate with NHS staff, because he’d rather scapegoat them for the crisis in the health service than take responsibility for his failure.”
Physician associate steamroll-out fiasco costs RCP President’s job; RCGP calls for halt

Dr Sarah Clarke, President of the Royal College of Physicians, bowed to the inevitable over the fiasco of physician associates expansion (as I predicted last week), and agreed to step down in September.
To the considerable surprise of absolutely nobody, the Royal College of GPs called for a halt to its members’ recruitment of PAs in general practice.
This came alongside the results of their survey of members on the subject of PAs, which has remarkable findings.
- 81% of all respondents said that they considered negative effects on patient safety to be one of the challenges of the use of PAs in general practice.
- 50% of all respondents reported being aware of specific examples of patient safety being compromised by the work of PAs, with common themes including misdiagnosis and diagnostic errors by PAs, inappropriate prescribing and management, and lack of communication to patients and GPs.
- 60% of all respondents with experience of working with PAs said that PAs in their practice act as the first point of contact for potentially serious conditions (falling to 48% of GP Partner respondents with experience of working with PAs).
- Only 25% of all respondents with experience of working with PAs said that all PAs had an annual appraisal (rising to 59% of GP Partner respondents with experience of working with PAs).
- 25% of all respondents with experience of working with PAs said that no time was scheduled for regular supervision of PAs, meaning PAs could only speak to their GP supervisor in gaps between appointments (rising to 31% of GP Partner respondents with experience of working with PAs).
- Even discounting the lack of regulation and the lack of adequate resources for training, induction and supervision, 24% of respondents said that they are aware of cases where the College’s 'red lines' are being breached.
Ooops.
👇@DrPhilBanfield has written to NHS West Yorkshire ICB about the damaging, misleading, unlawful ‘It’s a GP practice thing’ campaign. Local doctors raising concerns about the title “Physician” being applied to non-doctors since Feb ‘23 were systematically ignored. We need answers https://t.co/n6h1fFsJDY pic.twitter.com/lhPb0CW3A3
— The BMA (@TheBMA) June 17, 2024
In last week’s ‘Cut’, I highlighted the illegally misleading posters from Bradford District and Craven health and care partnership labelling a physician associate as ‘physician’. This letter from BMA chair Dr Phil Banfield to West Yorkshire ICB, copied to Victoria Atkins and NHSE chief exec Amanda Pritchard and MD Steve Powis asserts that local doctors have been complaining about the calling of PAs ‘physicians’ since February 2023: Dr Banfield’s letter did not, however, offer to provide documented proof of that claim.
It is quite tough to decide whether the Conservative And Unionist Party’s election campaign or the (now clearly doomed) attempt to steamroll-out the medical associate roles has been the bigger failure.
In both cases, one must have a heart of stone not to laugh.
The current attempt to steamroll-out the expansion of medical associate roles has blatantly failed. It’s over.
If those trying to achieve this think that the medical associate idea can work, then they’re going to need to take a completely different approach. One that takes the affected (in this case, medical) workforce with them.

And this can be done. Pharmacy technicians amply prove this.
Carrying on regardless with the steamroll-out of these roles in the absence of the medical profession’s tolerance is a strategy which we might note for its boldness more than commend for its wisdom.
The penny really needs to drop that the NHS medical workforce are no longer passively accepting bad conditions and unfair practices. The 2020s are here, and they want their terms and conditions back.
Thank you for asking me this question
— Dr Phil Hammond 💙 (@drphilhammond) June 21, 2024
I generally refrain from comparing medical scandals because they are all tragedies in their own way.
The Bristol heart scandal arose because the unit had demonstrably worse results for paediatric cardiac surgery than other units, but was… https://t.co/riGDhnQfCs
I strongly recommend reading Dr Phil Hammond’s wise reflections on this subject.
The Positive Professor rides again
Professor Karol Sikora is an oncologist, who used to work in the NHS more than twenty-five years ago. As far as can be seen, his last NHS job was at the Hammersmith in 1997 (he later held an honorary professor post at Imperial).
During the pandemic, he found a berth in the Daily Express as ‘The Positive Professor’, in which capacity he was consistently wrong about every significant aspect of dealing with the Covid19 pandemic.

You can’t keep a good man down: nor can you keep Professor Sikora down. He is back in the Boris Johnson Fanzine, to whine about the failure of his private chain of Rutherford Cancer Centres, by way of endorsing the Reform manifesto commitments on the NHS.
Once upon a time, free market people used to accept that private businesses went to the market and succeeded or failed on their own merits.
Now, we find Professor Sikora endorsing Reform’s approach to health policy. This is unsurprising: as my manifesto analysis showed, Reform plan to sling money at private sector providers as if there is no tomorrow (and indeed no limit on government borrowing).
The Reform manifesto stuff on health is very funny: its £17 billion annual price tag is a vast, vast underestimate of what it’d actually cost. And its stuff on pensions and social care has no costing against it.
I hate having to introduce reality to these wild fantasies, but the private sector has really quite little spare capacity.

As the man running the UK’s leading private hospital provider provider business recently stated.
Recommended and required reading
A short break from my arduous duties @HSJnews to work on an exciting project for the incoming government.
— Julian Patterson (@jtweeterson) June 20, 2024
Read about it here, including my prediction of the general election result.
Sorry @HPIAndyCowper but I'm doing punditry now - and I'm rarely wronghttps://t.co/Njh7BJNzhH
The fragrant Julian Patterson’s last pre-election HSJ column is A Triumph. As the late, great Leonard Cohen so nearly sang, “I have seen the future, and it’s purdah”.
The latest piece for the Kings Fund by the great Nick Timmins takes on the question How Likely Is A General Election To Transform Health And Social Care?
Healthcare technologist Jess Morley and colleagues’ new BMJ Informatics paper on ‘Promising algorithms to perilous applications: a systematic review of risk stratification tools for predicting healthcare utilisation’.
Jess Morley’s doctoral thesis, Designing an algorithmically enhanced NHS, is also now online.
Decent BBC News summary on why politicians aren’t talking about social care.
Economist coverage of the ransomware attack on a London NHS pathology provider.
Amusingly bad Boris Johnson Fanzine piece on why Reform’s manifesto commitment to subsidise private medical insurance is good, actually.