Cowper’s Cut 335: Summertime Blues

I won’t pretend that this has been the most action-packed week ever in English health policy and politics.

Of course, as the week unfurled, we saw gradual statement-making by national and representative bodies about the UK’s racist riots mentioned at the start of last week’s ‘Cut’, but relatively little that looks up to the scale of Partha Kar’s righteous critique.
How do you solve a problem like TPP?

It wasn’t, however, perhaps very surprising. Having asked around colleagues in the community sector, the best articulation of why this has happened is as follows: “the TPP system is probably the only one that can provide properly integrated care records (except for acute/emergency).
“In our region, GPs, community Trusts, care homes, hospices, district nurses, some schools, and even some hospital wards use SystmOne and are all fairly successfully linked together.
“The other providers are so stuck on protecting their little monopolies / oligopolies that they risk losing it all to TPP if the NHS starts commissioning at integrated levels. (And they’d deserve to lose it, because their products and services are shit.)”
It comes down to brass tacks: the TPP SystmOne product actually works, and can be used with other parts of the health economy. It shouldn’t need saying that interoperability ought to have been a top priority in what the NHS digitally commissions.
And it hasn’t.
This is why there’s a virtual lock-in to acute EPR systems, and why there is still a massive hit to acute trusts’ performance every time they implement an EPR. That is in a ‘marketplace’ where there are two main providers.
The price and the value of GP industrial action

Documents leaked to Health Service Journal’s James Illman reveal that NHS England’s modelling implies that the current work-to-rule by GP practices may cost the wider system £570 million over the coming four months.
That sum is “based on a 30 per cent reduction in GP activity from August to November … this includes more than a million extra A&E attendances, and nearly two million more pharmacy visits, as well as many extra calls to 111 and urgent care centre visits.
“NHSE’s modelling also includes a less severe scenario, where GPs reduce activity by 10 per cent for four months – but even under this scenario projected costs could hit around £205 million and nearly 250,000 extra referrals could be generated”.
Top Issue
The NHS and the economy have been scrapping for top spot in Ipsos’ long-running Issues Index study of UK public concerns.
The latest data set for July 2024 sees that of the polling respondents, “almost half (47%) identify healthcare as a concern, an increase of seven percentage points since June. This is the highest level of worry about the health service in the post COVID-19 pandemic era: the previous high was recorded at the time of the 2019 General Election in December (55%)”.
And Ipsos’ latest six-monthly dose of work for the Health Foundation has found that satisfaction with the NHS continues to decline. Since November 2023, it finds that “the public are less positive about the service the NHS provides … They are less likely to agree that their local NHS is providing them with a good service (down from 44% in in November 2023 to 37% in May 2024), or that the NHS is providing a good service nationally (down from 34% in November 2023 to 28% in May 2024).
“In line with November 2023, over half of the public continue to think the general standard of care provided by the NHS over the last 12 months has got worse (55%), and optimism about the future remains largely negative, with half (52%) also stating they think the standard of care will get worse over the next 12 months - in line with November 2023 (53%)”.

The Health Foundation’s write-up is here.
Waits and measures
The latest RTT data came out, covering the last full month period of Conservative And Unionist Party government (June 2024).
The total RTT waiting list grew by 20,000, to 7.62 million. There are 120 two-year waiters; 2,621 eighteen-month waiters (both supposed to have been long since gone); and fifteen-month waiters rose by 2,000 to 58,000 (this is th next millstone, sorry, milestone target).
75% of patients were admitted, transferred or discharged from A&E departments within four hours in July 2024 (slightly up from 74.6% in June and on the 74% from July 2023. There were 2.32 million attendances at A&Es across England in July 2024, and 552,468 emergency admissions. 119,409 patients who attended A&E were there for more than 12 hours in July (8.7% of all attendances): down from 135,901 (9.5%) in June and down from 96,260 (7.2%) in July 2023.
In June 2024, 76.3% of cancer patients were told they had cancer or had it definitively ruled out within 28 days, slightly down from 76.4% in May. This is against the target of 75%. This is up from 73.4% in June 2023. This is the 4th highest month since records began in 2021.
The backlog of cancer patients waiting over 62 days for week ending 30th June 2024 was 17,759. This is slightly up from 17,709 from week ending 2nd June 2024. This is down from last year – 21,631 for week ending 25th June 2023.

Rob Findlay’s HSJ analysis is here.
The state of medical education
The GMC’s annual report into the state of UK medical education and practice is, unsurprisingly, not full of good news.
Chronicling high levels of observed patient safety problems, burnout, trainer dissatisfaction and intentions to leave the profession, it finds that “41% report having seen patient safety compromised. Seeking to protect their wellbeing, doctors are taking matters into their own hands. Many are reducing their hours and declining additional work. A concerning proportion are taking time off due to stress. This further constrains capacity, increasing the pressure on those who remain …
“Doctors in training are now more likely to be at high risk of burnout than any other group. They are also among the most likely to be considering leaving the UK. Issues around rotas and frequent placement changes are disrupting family life and undermining the sense of belonging needed for a long, happy career …”
“Of all doctor groups, GPs continue to be the least likely to be satisfied and the most likely to be struggling with their workload. Support for their wellbeing is vital”.
This is stuff that members of the Paying Attention Community have known for some years. So what is the GMC’s solution?
Physician associates! “But so, too, is a fresh approach to the delivery of services. Developing the multi-disciplinary team in general practice will be crucial in freeing up doctors’ time to do what only they can do. Intelligently using the skills mix of the health workforce is key to increasing productivity and improving patient outcomes”.
Mmmmmmm.
The Alan comeback

Gosh, I bet you’ve missed The People’s Partridge’s happy, shining face.
But you can’t keep a good man down, and you can’t keep Alan down either.
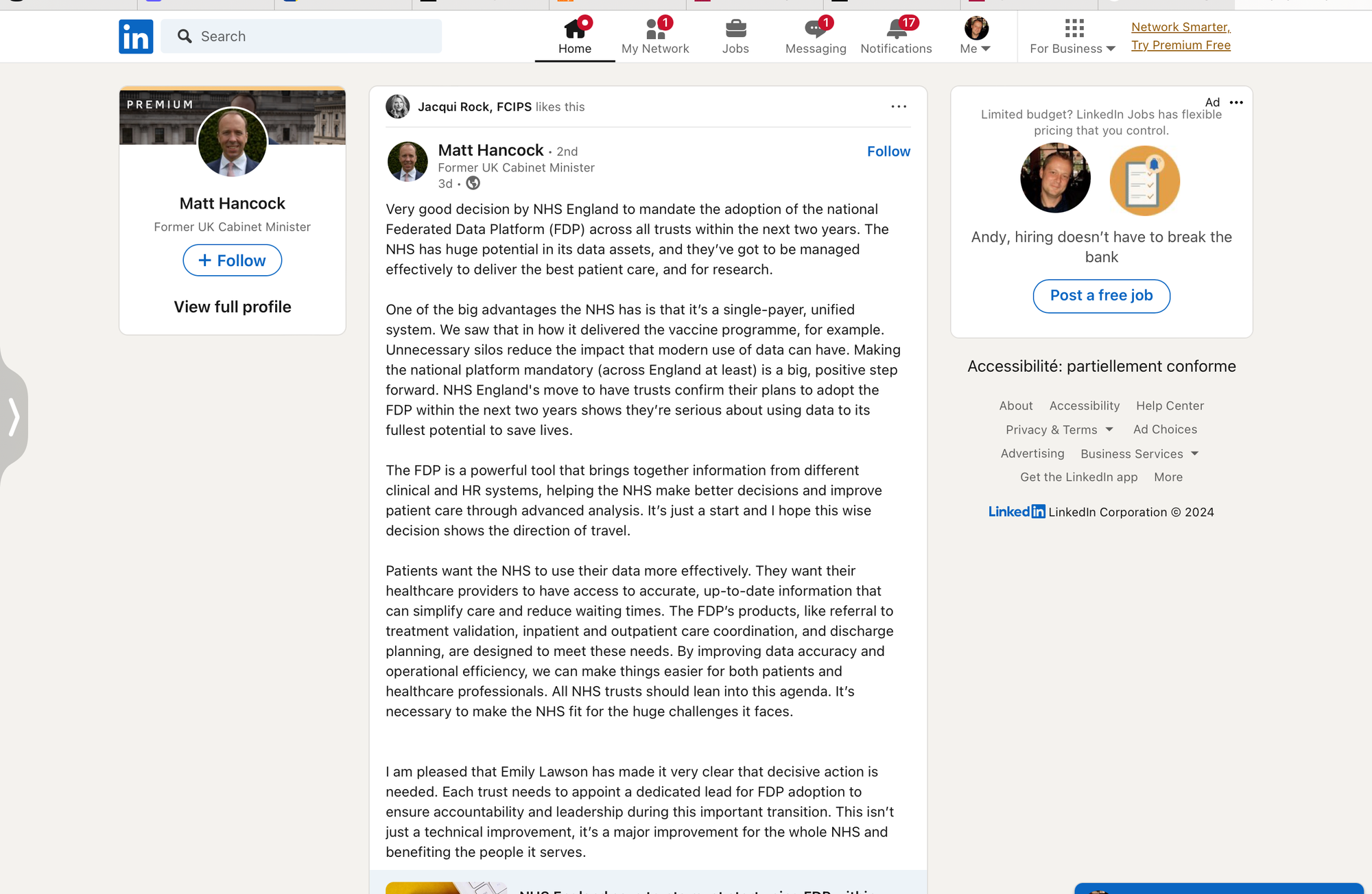
He’s been trumpeting the NHS England decision to make the adoption of the Federated Data Platform mandatory on his LinkedIn profile.
HSJ reported on this U-turn over making the Federated Data Platform mandatory last week. My usual COI declaration: I used to be a paid advisor to FDP contract winner Palantir, in which role I warned them repeatedly (but clearly to no avail) that effective FDP implementation was going to require proper communications and resourcing.
The FDP rollout has, unsurprisingly, not been going well, as I mentioned in ‘Cut’ just a few weeks ago: “it’s not a well-kept secret that the FDP rollout is underperforming both hopes and expectations. The roll-out is inconsistent in delivery and perceived support; some sites have found it hard to get their data onto the platform; there have been challenges with consent.
“There has been no standardisation of local data or of information governance. These are the absolute basics of architecture that you need for the foundation of digital reliability: they are notably absent.
“There has been over-complication at launch, and trying to do too much at once as opposed to launching a functional product and then extending from a reliable working base with a successful proof of concept.
“There is, frankly, a lack of trust.”
It is typical of the sheer brilliance of NHS England in ignoring the massive evidence that nationally making programmes mandatory does not have great outcomes for those programmes’ sustainability.
Let us consider, by way of example, just how brilliantly NHS England’s incentivisation of financial lying in ICS budgets has gone.

That’s been a Major Triumph, I’m sure you’ll agree.
Anyway, happy birthday to me: 53 years young today. (No, I agree: I don’t look a day over 52 3/4.)
Recommended and required reading

In the Haywood Quarterly, Tamara Finkelstein (head of the Government Policy Profession) asks whether it’s time for Civil Service generalists to become part of a profession. (Yes, it clearly is.)
BMJ Investigation piece by the excellent Deb Cohen and Margaret McCartney looks at the evidence for Grail’s ‘Galleri’ blood test for cancer, and finds that “serious concerns” by the independent National Screening Committee were ignored; suggests that evidence of Galleri’s lack of effectiveness was ignored before the commercial deal was done; and flags up a class action lawsuit claiming that Grail exaggerated Galleri’s effectiveness in order to increase their share price.
I seem to have missed Insource director Rob Findlay’s excellent 2019 presentation to the Royal College of Emergency Medicine on bed occupancy.
FT piece on the rise in rates of cancer among young people.
Steve Black’s latest HSJ column gives the argument for abolishing the Care Quality Commission.
Dr Hilary Cass’ letter to NHS England’s specialised commissioning leads detailing serious concerns about NHS-commissioned adult gender clinics has been published.
Do women make better doctors than men? Yes, slightly, studies show.
Interesting if slightly confused Observer piece on at-home testing.





