Cowper’s Cut 353: Into winter
Having spent most of last week’s column writing about Labour’s evident lack of a health policy that confronts the need for trade-offs, you could have knocked me down with a copy of Matt Hancock’s ‘Pandemic Diarrhoea’ (many of which remain available if you need a Christmas present for someone you truly detest) when this week started with Secretary Of State For Health But Social Care Wes Streeting not only making a clear decision about a major trade-off, but also doing so in public.

SOS Streeting briefed the national media that “we're seeing record pressures on services as we move into December. I want to see patient safety prioritised as we brace ourselves for the coming months. I'm asking trusts to focus on ambulance delays, handovers and the longest A&E waits."
This is good, necessary prioritisation. Mr Streeting deserves congratulation for being clear that safety comes before target-chasing.
To a large extent, making this explicit trade-off is just acknowledging reality, but the national leadership of the English NHS has been so poor at doing this over the past few years that we should acknowledge it as a revolutionary act.

There was, for most trusts, no realistic chance of hitting the A&E 4-hour target given the huge rise in flu and other seasonal disease cases. Currently, ambulance handovers are almost double their rate from 2023, which was itself not great. The change for this year’s flu vaccination start date from September to October will doubtless be scrutinised: there has also been low vaccination take-up in very young children.

It’s also quite possible that Mr Streeting is remembering NHS England’s tragicomic flailing-about back in March 2024, ordering provider chief executives to hit the A&E monthly target or risk financial cuts. If SOS Streeting or his team pay attention to receipts such as this, then The Woman In Black Amanda Pritchard’s tenure as NHSE chief executive might not see summer 2025.
The outbreak of reality didn’t prevent some vigorous yet anonymous pushback getting into the Financial Times.
Patient safety back in vogue for the Winter 24-25 Collection
Emphasis on patient safety, like Sergeant Pepper’s Lonely Hearts Club Band, just keeps going in and out of style in English health policy and politics.

A new report from the Institute for Global Health Innovation, Lord Darzi’s Imperial mob (funded by Jeremy Hunt’s Patient Safety Watch) looks at the National State Of Patient Safety 2024.
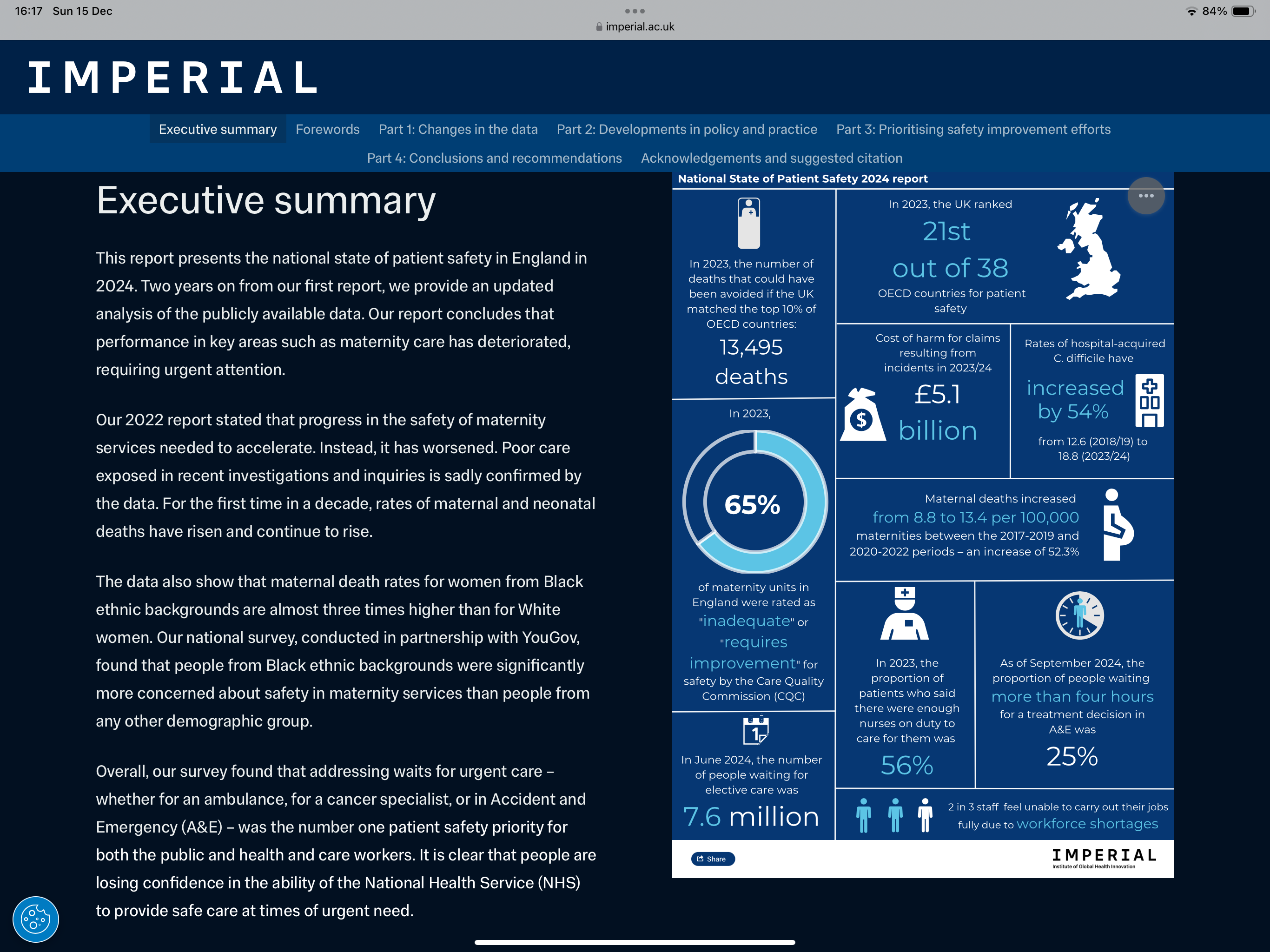
Its findings are not pretty. Nor are they surprising.
The report finds that “adverse effects of medical treatment, which led to death or disability, was twice as high in the North East of England than in Greater London. The North of England also had the highest proportion of hospital trusts with a greater than expected number of deaths – a figure that has increased from 8% to 14% since our last report.
“The human, societal and economic cost of clinical harm is considerable, and growing. Based on work by the Organisation for Economic Co-operation and Development (OECD), the costs of unsafe care in England can be conservatively estimated at £14.7 billion per year. This figure excludes the indirect impact of harm, such as on people’s quality of life and ability to work, and the rising costs of clinical negligence claims.”
Its two main recommendations are
- Local NHS organisations must be supported to adopt evidence-based interventions to tackle the most common safety problems causing significant harm to patients. Our analysis of trust patient safety plans identified six common problems that many organisations are tackling, such as pressure ulcers and patient falls.
Adopting proven interventions to common problems like these would finally see the NHS truly acting like a National Health Service. We envisage a future where the first port of call for NHS organisations is a repository of such interventions, along with the support they need to implement them, rather than developing their own solutions from scratch. - National organisations must agree on a focused set of patient safety improvement priorities for the system to rally around. Our analysis found a crowded landscape of patient safety bodies, an opaque process for national priority setting, and evidence that the system cannot keep pace with the volume of recommendations it receives.
We envisage a future where patients and healthcare workers are partners in the development of these priorities, and where national organisations rationalise their own activities to ensure the NHS is supported to deliver improvements against them.
Yep, that sounds pretty fair - if a bit in the ‘God is love’ / ‘Please adjust your dress before leaving’ vein.
It remains to be seen whether the English NHS’s epically confusing and fragmented responsibility for patient safety will be up to incentivising either of these to happen, though.
NHS financial lying to be banned (sort of)

Long-time readers need scant reminding that in ‘Cowper’s Cut’ and elsewhere, I have been banging on about financial lying in the NHS for years.
This is interesting, but it is ‘Not News’ to members of the Paying Attention Community.
— Andy Cowper (@HPIAndyCowper) May 28, 2024
NHS England has been incentivising financial lying for a long time.
The chickens are just coming home to roost. And possibly to roast. https://t.co/JTfdOjyZGp
In this thread from May 2024 on Kiss (formerly Twitter), I concluded a series of examples on NHS England’s blatant incentivisation of financial lying with the comment that “I keep going on about NHS England’s leadership being crap. And there is a reason for this: they are crap”.
Sometimes, you just need Occam’s Razor.

Anyway, Health Service Journal’s Zoe Tidman noted this week that “the government said it would no longer allow capital raids to fund pay awards across the entire public sector, in evidence to the pay review bodies this week.
“The evidence said: “The government has changed the fiscal rules to remove the incentive to make these kinds of switches, and will be changing the consolidated budgeting guidance to explicitly rule them out.” It said the move meant departments will have to live within their means.
“However, HSJ understands the fiscal change will affect capital budget raids to fund pressures beyond just pay, and prevent the practice where capital budgets are reduced with the intention of covering revenue gaps.”
NHS financial liar-in-chief comes to repentance (maybe)

As if this week’s events were not already sufficiently remarkable, NHS England’s national director of finance Julian Kelly (who oversaw much of the aforementioned incentivisation of financial lying) told members of the frankly incredulous NHS financial community that the 2025-6 mantra is ‘keep it real’.
No, seriously. HSJ’s Henry Anderson spotted that at the Healthcare Financial Managers’ Association’s recent conference, Mr Kelly had urged “greater realism from local leaders in next year’s financial planning round, warning they must urgently make “difficult” choices about what they can deliver with what will “feel like a real terms cut”.”

Well.
(To be fair, Mr Kelly could scarcely have urged FDs towards less realism, given his on-the-record conduct.)
Tongue heroically far in his cheek, Mr Kelly also said local finance directors must “be realistic” about funding in 2025-6 … and accept there are “some really properly important and difficult conversations for us to have and we are going to need to get into them fast”.
On 2025-6 preparation, he told them, “in the context where it’ll feel like, on average, a real terms cut in sort of activity spending power [that means] people coming back quickly, not with ‘I need billions more’, but, ‘this is what I think we can do’.” One must have a heart of stone not to laugh.
Mr Kelly also said it was likely the elective recovery fund would be capped next year.

Let’s segue to Milton Keynes chief executive Joe Harrison’s comments to the provider trust’s November board meeting about the costs associated with efforts to clear the number of long-waiting patients, as picked up by Zoe Tidman of HSJ.
Harrison said that the trust was carrying out extra work on evenings and weekends to treat these patients and contracting external providers to help, but noted for the record that “the tariff the organisation gets paid is insufficient to cover the total cost of that premium activity.
“And so at some point, we will have to have a conversation about whether we can continue with premium activity and continue to reduce longer waiters, versus the … impact on our financial plan.”
And HSJ’s Alison Moore noted that NHS spending on agency and bank shifts for doctors rose by £470 million to exceed £3 billion last year – 68 per cent up on pre-covid levels.
Performance data: it’s not great news
Ooops.
The latest RTT backlog data and the next dose of Winter SitRep dropped this week, and you know what? It’s not great.
There was a drop in the total RTT list, from 7.6 million to 7.5 million. The NHS is supposed to be hitting 15 months, but 20,930 people aren’t getting that.
There were an average of 1,861 patients in hospital with flu each day last week, up 69% from 1,099 the previous week; an average of 1,015 adult beds were closed due to patients in hospital with diarrhoea and vomiting or norovirus-like symptoms last week, up 13% week-on-week from 901.
There were 2.31 million attendances at A&Es across England in November, making it the busiest November on record. 35.8% of ambulance handover delays took longer than 30 minutes (up from 33.8% in the same period last year); around 16.3% of handover delays were longer than an hour, up from 15.2% last year.

As ever, Dr Rob Findlay of Insource offers peerless RTT analysis in HSJ.

The Times picked this up for a lengthy news analysis by Eleanor Hayward and George Willoughby.
Stevens: don’t fuck about with my mental health standard
I mentioned in last week’s column Lord Stevens of Birmingham’s Lords speech on the proposals in draft legislation to weaken the mental health investment standard: the funding escalation mechanism that he left in place.
Working with both Opposition front bench parties in the Lords and various crossbench peers, NHS England’s former chief executive has now tabled a number of amendments.
It would be quite awkward for Labour MPs in the Commons to vote to facilitate the cutting of spending on mental health in English national aggregate. One to watch.
Recommended and required reading
A genuinely fascinating read: ‘The NHS Internal Market: transcript of a witness seminar held at the University of Liverpool in London on 5 December 2017’.
More weight loss drugs hype in this Financial Times long read. Are GLP-1 receptor agonists the new AI - a universal panacea? And as if by magic, you’ll never guess which former PM’s Institute is hyping them …
New Innovation Ecosystem Programme report by Roland Sinker (chief executive of Cambridge University Hospitals NHS FT and Cambridge Biomedical Campus) claims that patients may miss out on the benefits of new technologies and new medical devices launches are being stymied because of regulatory hurdles and poor alignment. Staff across the NHS lack the capacity and support needed to “test, adopt and scale” innovation, says the report commissioned by NHS England.
New LSE study in The Lancet suggests that based on data from 2000-2020, NICE might be costing more lives than it saves: a very interesting finding (and therefore probably wrong).
Wes Streeting hagiography in The Times.
Trouble ahead: the FT reports that the Treasury Munchkins are not feeling generous ahead of the next public sector pay round.
Execrable ‘why-oh-why’ Jeremiad in the Boris Johnson Fanzine about the Priory Group: you’ll be surprised to hear that the piece implies that its poor patient safety record is the NHS’s fault …
Convicted serial child killer Lucy Letby’s legal team are trailing the release of new evidence on Monday, which they believe undermines her convictions.
Former GSK chief executive Andrew Witty is now chief executive of United Health Group, and wrote this essay about US healthcare for the New York Times following the murder of United Healthcare chief executive Brian Thompson in New York.
Can Covid Clawback Commissioner claw cash?
Nice BBC News story about Slade’s ‘Merry Christmas Everybody’ singer and songwriter Noddy Holder’s successful cancer treatment.










