Cowper’s Cut 362: The Penny officially drops in Amandaland
To the considerable surprise of absolutely no readers of ‘Cowper’s Cut’, Dr Penny Dash was announced as the preferred candidate to be the next chair of Amandaland (the artist formerly known as NHS England).

Romantically enough, this was made public on Valentine’s Day.
What does it mean from our NHS-hearting English nation, now that The Penny has officially dropped? How will it improve people’s healthcare?
Opinions about the significance of Dr Dash’s arrival vary, as she is well aware. Her lengthy period of service at management consultancy McKinseys is a red flag to those people who think that management consultancies have added scant value to the NHS: these people do have the recent academic literature on their side.
Those who are more supportive point out that she took on the unrewarding task of chairing North-West London Integrated Care Board at a time when that system (like most systems) faced no small amount of challenges, and appears broadly to have done a decent job.
The pro- and anti-camps are one fairly unsurprising aspect of this: the broader circumstances and shifting political sands into which Dr Dash will be landing as Amandaland’s new chair are another.
Her confirmation hearing with the Health Select Committee could be quite a decent watch: for some clues, have a look at her comments to the Institute For Government event from November 2024 (from eight minutes in).
Among the critical constraints on improving the NHS in England will be Dr Dash’s relationship with the chief executive of Amandaland.
Speaking of which …
The Woman In Black on PFI’s return (The One In Which Amanda Pritchard Kicks Bishop Brennan Up The Arse)
This Thursday, NHS England’s chief executive The Woman In Black Amanda Pritchard did something very out-of-character: she went on national media, and actually Said Something Interesting.

She told BBC Radio Four’s ‘Today’ programme (as Health Service Journal kindly transcribed) that “the government have given more capital to the NHS this year, which is hugely welcome, but in the current financial context we can’t keep asking the government for more state funding. We are not going to fill the gap that way … we need to think much more radically, particularly about capital.
“I think we must consider private capital investment in the NHS.
“If we don’t fix our buildings, if we don’t fix our technology, we are not going to get to a place where we can really drive that long-term improvement.”
This followed a new report from NHS Confederation, advocating for neo-PFI.
As readers know, I recently had a go at the capital piece in this column.

New FOI-based work from the Liberal Democrat’s this week given to The Guardian also revealed a likely cost of £5.7 billion for patching up some of the New (If Fictional) Hospitals in order for them to remain functional prior to their demolition for rebuilds or replacements.
So, whether it was me, the Lib Dems, the Confed report, or the Financial Times’ shocking recent piece on the state of QMC Nottingham’s hospital estate, something in the ether made Amandaland think that Something Must Be Done about the longstanding NHS capital drought caused by NHS England to give the appearance of balancing the books financially.
And PFI is, indeed, Something.
Let us reflect on how this happened. The idea that Amanda Pritchard went pro-PFI freelancing off her own bat will find few takers outside the Hard Of Thought Community. It is - just barely - conceivable that The Woman In Black has read the writing on the career wall and decided that if she’s going out, then she might as well do something useful as she leaves.
It is, however, unlikely. A fiscal-policy-freelancing Woman In Black would be the equivalent of the ‘Father Ted’ episode (number 6, series 3) in which our bet-losing hero is charged with the task of ‘Kicking Bishop Brennan Up The Arse’.
So we move to the next sensible question: who authorised her to do this?
From that, we can work out why.
Given the Treasury Headlock over public sector fiscal decisions (and neo-PFI is one such), then defying Treasury orthodoxy in this way requires a certain political unassailability.

Now, who do we know who used to be stationed in Amandaland, and now works at 10 Downing Street?
‘Don’t let’s be beastly to Amanda!’

This would tie in reasonably well with the bathos-drenched Guardian editorial this week, saying ‘don’t let’s be beastly to Amanda!’

One must have a heart of stone not to laugh at this … even if one were to ignore The Guardian’s attempted health political futurology of recent times. Bless Denis: he never changes.
The piece itself? Genuinely (albeit unintentionally) funny.
It claims of new NHSE chair Dr Dash and DHSC permanent secretary (no idea) that “the filling of these two vacant posts means Ms Pritchard is likely to find she has less room to manoeuvre; the high level of autonomy granted to NHS England by the Conservatives is in the process of being reduced.”
This analysis is impressively wrong. The ‘more Matt Hancock’ clauses in the 2022 Health And Care Act effectively handed control of NHS England back very, very firmly to the Health Secretary.

I showed this when I published my analysis alongside the leak of the White Paper back in 2021.
Also funny: “NHS England’s structure (with its 42 integrated care boards) is still bedding in”. Fair to observe that NHSE’s structure has had bits folded in to it (Monitor, TDA, Health Education England, NHS Digital, NHS Kiss) and there have been some NHSE redundancies made with more coming, but the 42 ICBs are not part of Amandaland.
This litany of the ill-informed chunters on: “another dynamic sees ICBs – with their duties to improve public health in partnership with councils – competing with big hospital trusts for influence and resources. One view of Ms Pritchard’s difficulties is that she is caught in the middle.”
This notion is - not wanting to blind anybody with health policy technical jargon - complete and utter bullshit. There is no such competition: providers are powerful, well-resourced, and understood by the Treasury - and so, as usual, they win.
Finally, it bids that “undermining NHS leaders also carries risks”.
Well, it might do if The Woman In Black Amanda Pritchard were the NHS’s leader. But it is wholly clear to anyone who knows what they’re talking about that Health But Social Care Secretary Wes Streeting is firmly and squarely in charge, and calling all the shots.
This is why he co-hosts the NHSE chief executive webinars when anything material is announced.
Still, apart from that, it was a really excellent piece. Valuable, too: I laughed until I stopped.
Productivity: a thing, apparently

The latest quarterly data from the Office For National Statistics on public sector productivity found more gloomy news about NHS performance.
These official figures in development found that “healthcare productivity was estimated to be 2.4% lower in Quarter 3 2024, compared with Quarter 3 2023. The decreases were caused by a larger growth in inputs than the growth in output for both total productivity and healthcare productivity.
“Healthcare productivity grew by an estimated 0.2% in Quarter 3 2024, compared with Quarter 2 2024; this follows a fall of 0.9% in Quarter 2 2024 … healthcare productivity is estimated to be 18.5% below its pre-pandemic peak in Quarter 4 2019.”
Now of course this depends how you measure the inputs and outputs, and Amandaland’s own work on NHS productivity is rather more flattering.
Amandaland and the ONS share a joint

Helpfully, the ONS and Amandaland issued this joint blog on what the data says.
Max Warner of the Institute for Fiscal Studies made this series of shrewd observations about this subject on BlueSky (what do you mean, you’re not there yet!), and these about the Amandaland/ONS joint blog.
Max is even-handed, but concludes, “there are two remaining questions. First, was ONS right to publish these estimates on such an important and high-profile issue when in places they are using worse estimates than what NHSE use, and what they themselves use for their annual estimates?
“Second, this confirms that NHSE is in a better position to measure many aspects of productivity. But is it desirable to have NHSE marking their own homework? Institutionally, it’s great that ONS are also trying to do this too, and are trying to improve their methodology.”
Nuffield Trust on the money
Guess what? It’s not so great. “NHS provider trusts reported a £1.2 billion overspend last year, amounting to 0.9% of income in 2023/24. This was a worse performance than the £448 million overspend the previous year, and significantly worse than the modest financial surpluses seen in 2020/21 and 2021/22 (putting the sector in a similar overall position to 2019/20, when financial instability left it poorly equipped to deal with the pandemic).
“This means that the sector has experienced the longest and steepest decline in its financial health since 2015/16, when it faced a £2.2 billion overspend largely concentrated in the acute hospital sector.
“While not as high as that £2.2 billion overspend in 2015/16, which amounted to 2.9% of income, this time overspends are spread across acute, ambulance and mental health trusts. Acute trusts still have the deepest overall overspends, but specialist, ambulance and mental health providers have also seen significant deterioration in recent years.”
Ooops.
And it looks as bad as it does compared to last financial year because of … PFI!
“In the most recent financial year (2023/24), trust accounts were affected by a new accountancy change – essentially the adoption of a new international accountancy standard. This is designed to better reflect the long-term liabilities that trusts with private finance initiative (PFI) and PFI-like arrangements for physical assets such as hospital buildings face.”
But clearly that was back in the olden days of Bad PFI, and now we will only have Good PFI. It’s like Bad AIDS and Good AIDS: keep up!
It was given exclusive page/screentime in the Financial Times.

For another good perspective on these issues in context, I recommend HSJ’s Henry Anderson’s latest ‘Following The Money’ column.
Who’s been NHS England chair these past three years?

Richard Meddings may perhaps have tried jolly hard in his time as chair of NHSE England, but his exit interview with the Sunday Times last week was highly irritating.
It was yet another embarrassing example of ‘Senior Healthcare Job Exit Logorrhea Syndrome’, particularly on the subject of the deep inadequacy of capital spending in the English NHS. Surprisingly, Mr Meddings found this surprising.
“I can’t remember the number of incidents we’ve had where we’ve actually closed operating theatres or wards because they’ve become unsafe. You’ve got some hospitals where you’ve got sewage coming up through the washbasins. It cannot be like this.
“It has been underinvested in, steadily, for years and years. It’s not a particular governmental issue — it’s across governments, across many years — and you have to see it to believe it”. One must have a heart of stone not to laugh at this insight.
Almost as funny was his attempt to defuse the Commons Public Accounts Committee’s criticism of NHS England’s leadership’s “remarkable complacency … the scale of government’s ambitions is great but senior officials do not seem to have ideas, or the drive, to match the level of change required.”
This was perhaps the most serious official public criticism of NHS senior management that I’ve seen in over a quarter of a century of writing about the NHS in England. (God, that makes me feel old.)
NHS England are still keeping us waiting for their promised detailed rebuttal of the “factual inaccuracies and flawed understanding” of the PAC charges, unless this defence by Meddings is all we get. If so, the bathos is magnificent: he reportedly felt its findings were “misguided” and “unfair. I don’t see any complacency whatsoever,” he said. Mr Meddings further described The Woman In Black, NHSE boss Amanda Pritchard, as “extremely pragmatic”.
Ahem.
Ten-Year Plan update
I went to the Cambridge Health Network event on the 10-Year Plan this week.
A few photos and rough notes follow below the ‘recommended and required reading’ section. General thoughts: it means well. They are trying hard.
But. Among the evening’s more remarkable assertions were Paul Corrigan’s that “there is no real cost of NHS capital”, which made those attending who had provider experience more than slightly surprised.
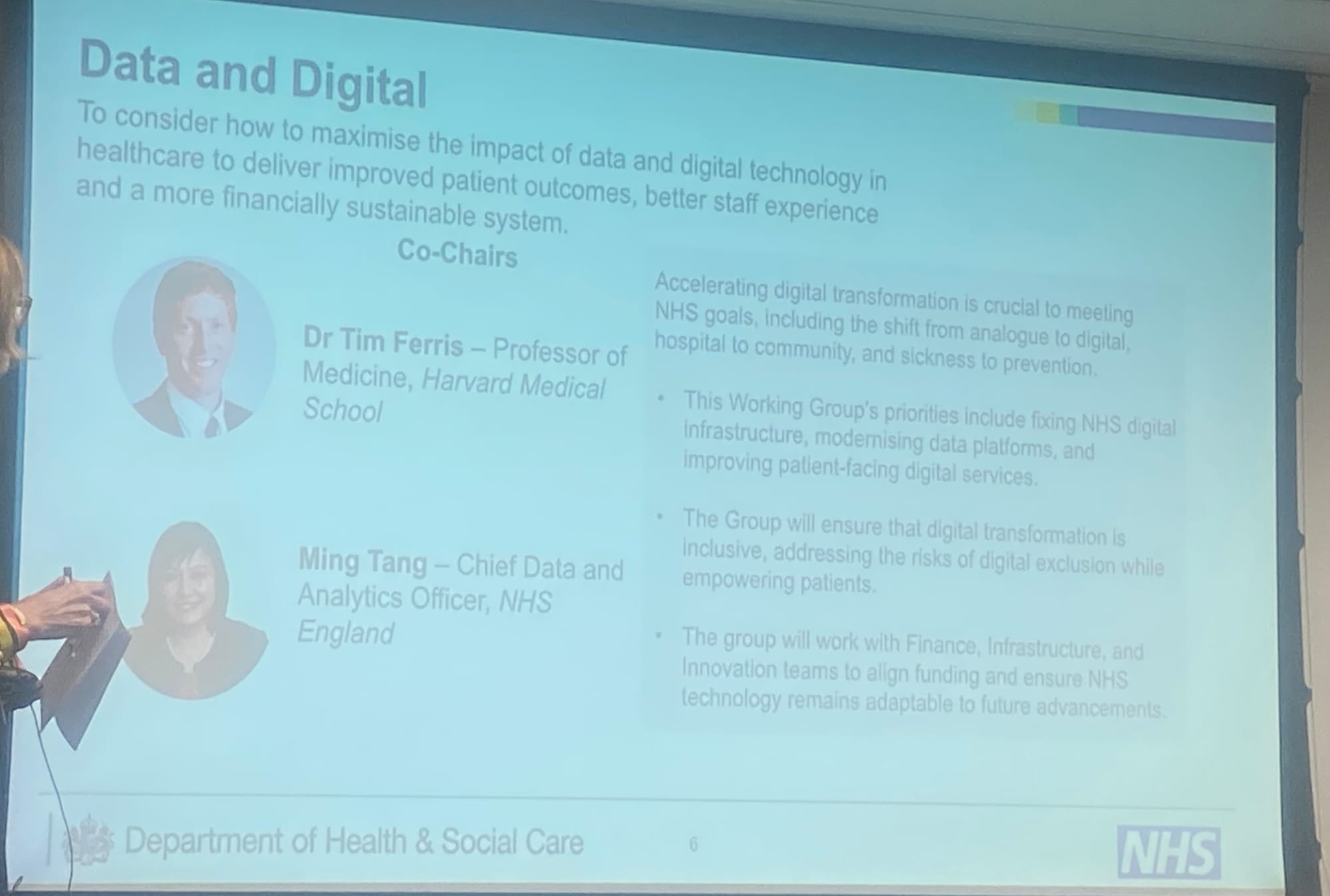
The only draft section that’s been leaked to me so far is the ‘data and digital’ one. It’s fine on the surface, but not very deeply between the lines, there is a remarkably concerning subtextual inference that a single provider would be A Good Thing.
The history of digital suggests strongly that it clearly wouldn’t be any such thing. A single patient records, and a single national set of standards on openness and interoperability would be a very good thing.
But having a single provider in the name of interoperability would be creating an unassailable monopoly: the water industry’s travails suggest strongly that we might want to avoid that at all costs.
(Do feel free to leak me any other draft 10YP sections that you might have: andycowper@hotmail.com)
Recommended and required reading
One of my regular clients is the data and software company RL Datix: I recorded this podcast for them with Will Browne of Emrys Health - one of the health data world’s upcoming bright young things.

Mike Farrar has been appointed interim Permanent Secretary of the Department of Health in Northern Ireland. That’s a very strong choice for a very troubled health system.
The Sunday Times has this story of another horrendous maternity service failure, again at Nottingham, compounded by provider and CQC failure. The cult of natural childbirth at all costs has a lot for which to answer.
The Times picked up on comments by the Information Commissioner John Edwards that patient confidentiality and data protection should not be routinely used to block reports into mental health homicides: it refers specifically to the Nottinghamshire triple homicide.
The Guardian has this piece on another potential development in cancer treatment.
Ten years ago, HSJ published a report that I wrote sponsored by Allocate Software on patient safety. Thank goodness that completely solved the problem.
Ten-Year Plan slides and notes
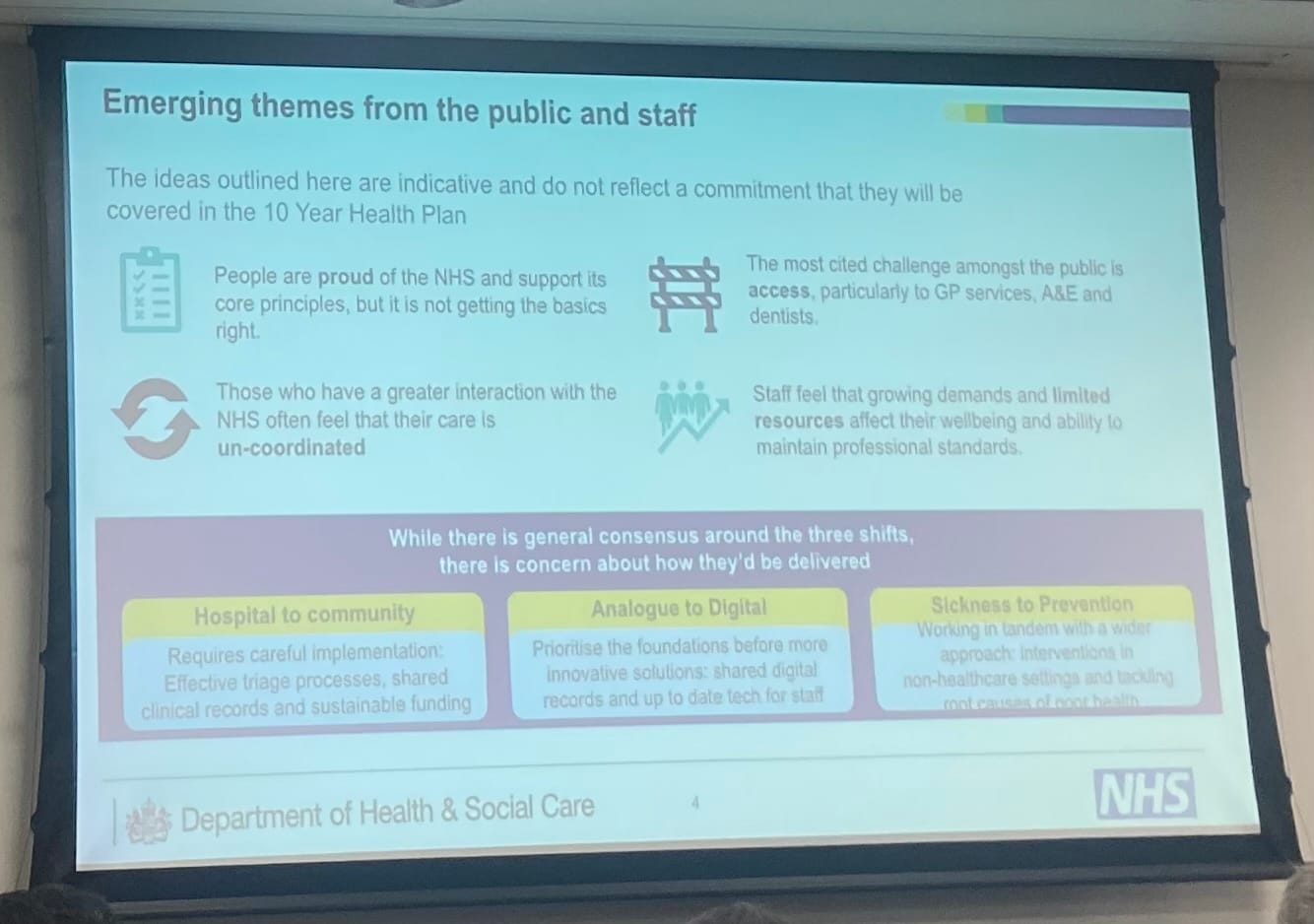
CHN 10 Year Plan event Feb 25
Count Tancredi from The Leopard “for everything to stay as it is, everything will have to change”
Sally Warren: SOS asked us not just for a plan but for a new process. The process is as important as the plan itself.
We got some entertaining suggestions, including Wes Streeting being replaced by Larry The Cat. Wes originally found this quite funny, until the PM mentioned it in Cabinet.
Public still think hospitals are still the safest place to be treated: many of us know that this is not true.
Paul Corrigan: When I was growing up, the state owned my house, education and health, which was wonderful until it wasn’t. It seemed fine till I was 18 and went to LSE, and wanted to own my education.
The public sector world of 2025 needs a critique of the historical social democratic promise and how it is fulfilled.
Part of vision. Taken from 2014 National Voices ‘I’ statements - incredibly moderate, but the NHS found it impossible to deliver them.
If you want to do something quite simple, lots of things need to change.
It would transform a lot of things if people were better at self-management. It is not ideological, but materially essential for the future of the NHS. Tech activation has changed many sectors of life: not got there on health. Tech has become a way in which we increasingly live our lives, but not in how the NHS runs. And I mean moderately old tech, like the mobile phones we have in our pockets - they’d be interesting to use in health services.
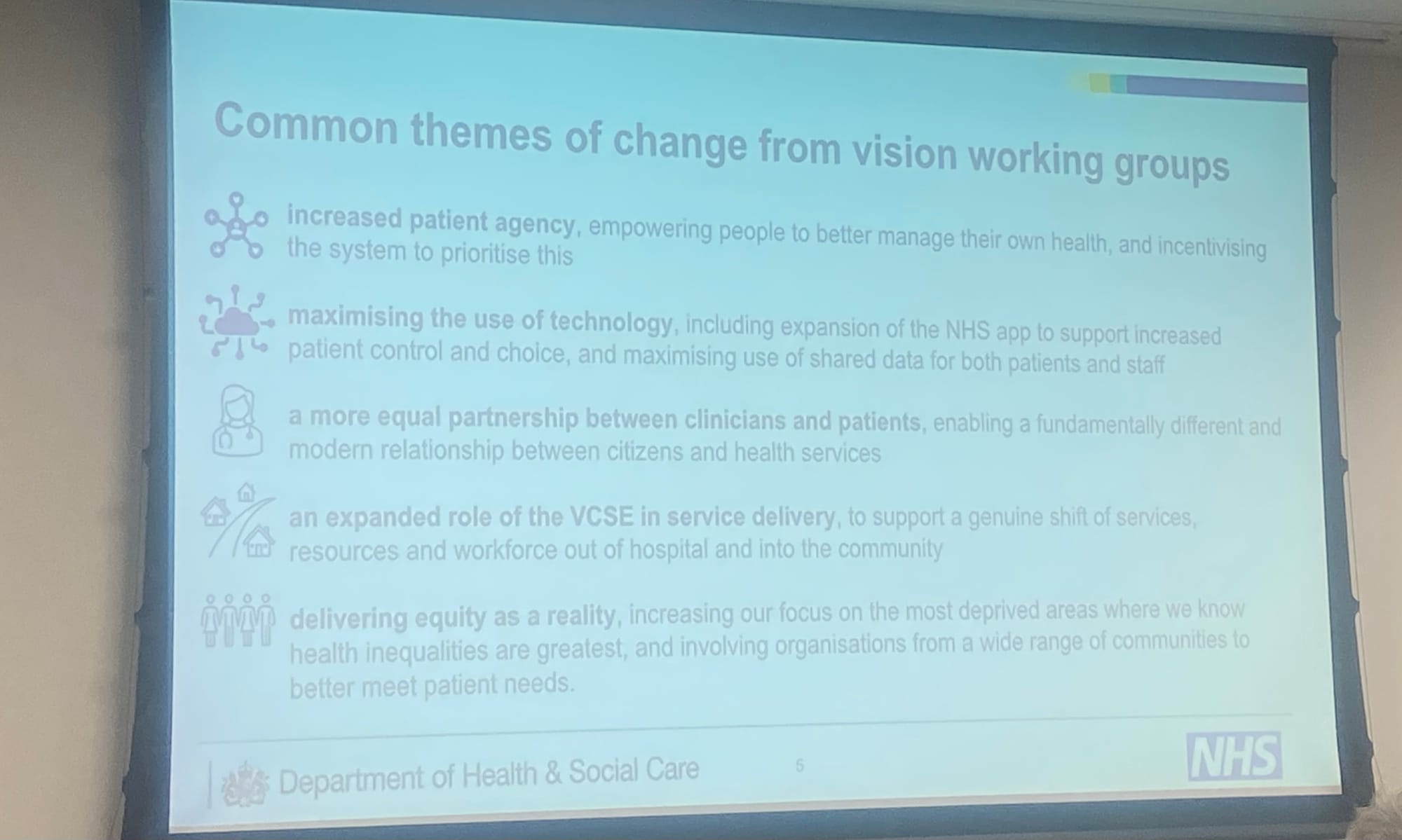
The next stage has to be about mobilising patient activation.
There will be a partnership with clinicians - how we make that work and mobilise patients. It’s in most clinicians’ interests to mobilise patients. How they get help to do that is essential. Crucial thing about our health services is the ecosystem of which it is a part: not the health system itself. How we get the NHS to relate to other private services, and the community and voluntary sectors is key. If the NHS goes on believing that it is making the weather in the health and care ecosystem, then it will be in a bad place in ten years time.
Let’s try to get to equity as a reality, not a nice-to-have. In 1948, Nye Bevan had the idea for equal access for all: it might be time to start doing it.
Data and digital
Paul Corrigan: NHS pretty poor partner and customer for medtech. Way we pay for tech is pocket-money approach. Sometimes used on deficits. Diff financial flows, not just for tech but for finance for tech.
Paul Corrigan: there is going to be now new resource apart from the patients. A materialist issue, not an ideological one.
Tim Ferris claims that tech firms do not look at savings to NHS in their costing model and so look at making 90% profit.
TPP (System One): £83 million turnover, £69 million profit
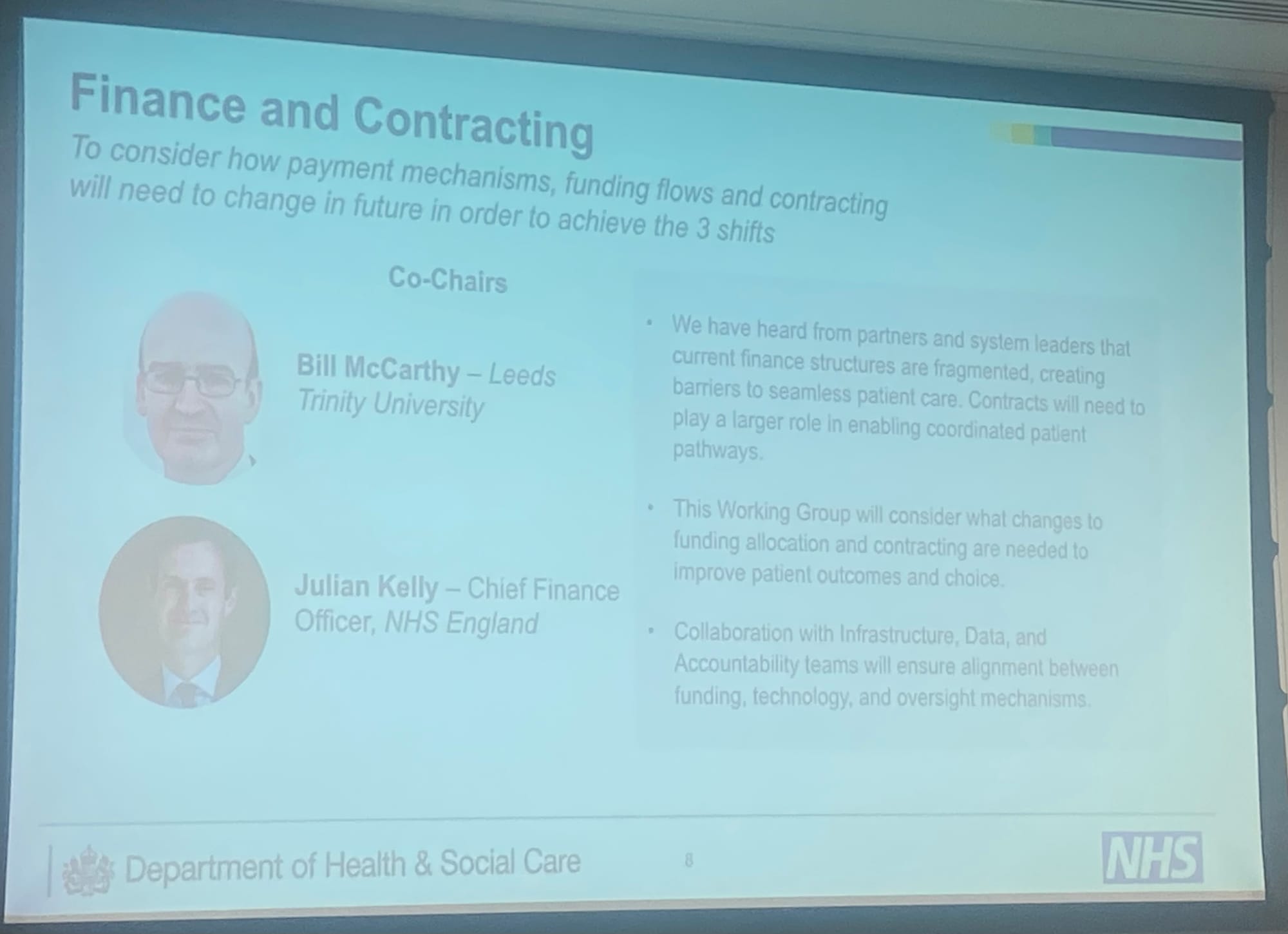
Finance
Paul Corrigan: If we don’t stop the NHS doing old things, we won’t be able to do new things. NHS never gets rid of anything which is incredibly inefficient. We all need to get rid of old stuff. There are sets of skills in doing this, which we need to learn.
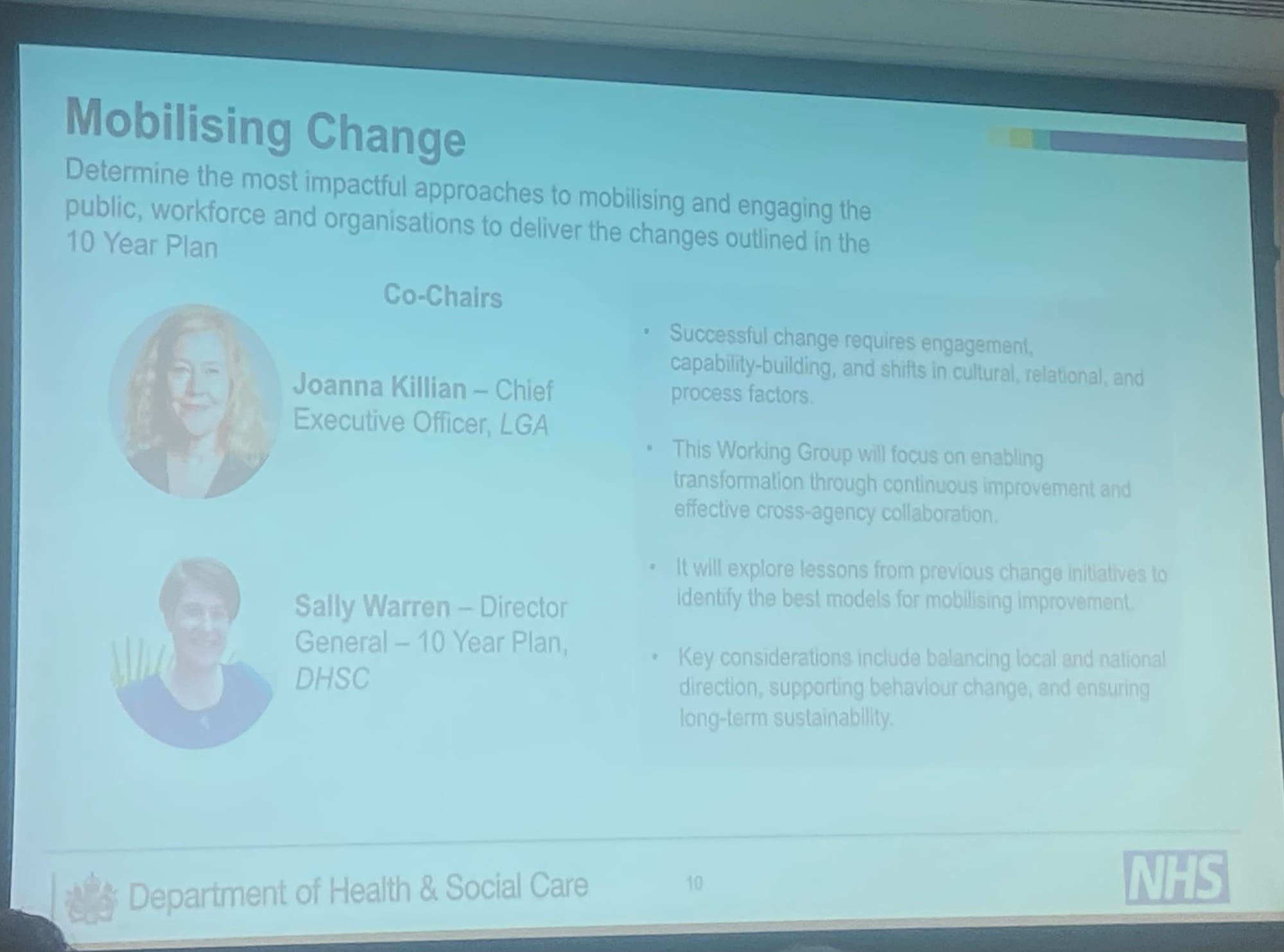
Mobilising change
Bob Klaber: we are weak on agency and understanding of agency, change culture riddled with bullying, hierarchy and paternalistic behaviour, Google Project Aristotle. Julia Unwin’s work on the rational and the relational - healthcare is a people business, co-producing outcomes that matter to people. We dictate process after process after process. If we’re serious about prevention, it is about deeply understanding agency.